Americans are in a lot of pain.
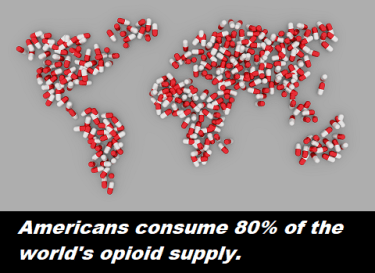
As a nation, we consume far more opioids than any other country on the planet. In fact, we consumer 80% of the global supply. That’s a lot – particularly for a country that comprises only 5% of the world population.
And if you include Canada and Western Europe, that figure increases to 95%. Opioid use, it seems, is a “First World issue.”
 In most countries, the use of opioid prescriptions is limited to acute hospitalization and trauma. Such as burns, surgery, childbirth and end-of-life care. And more than 70% of the world’s population actually live in countries where there is no access to opioids.
In most countries, the use of opioid prescriptions is limited to acute hospitalization and trauma. Such as burns, surgery, childbirth and end-of-life care. And more than 70% of the world’s population actually live in countries where there is no access to opioids.
Why Does It Still Hurt?
With so much access to pain medication, you might assume that Americans are beginning to feel less pain. You would be wrong.
The most recent studies show that Americans generally report higher levels of chronic pain than they did before the drug abuse epidemic started. In fact, there is simply no concrete evidence that opioid painkillers can effectively treat long-term chronic pain.
That’s basically because of increased tolerance to the drugs. Stanford psychiatrist Anna Lembke, author of Drug Dealer, MD, explains:
It’s absolutely true that, if you were to get opioids for your pain, it would be like a magical cure for about a month or maybe two. But after a while, there’s a very high likelihood that they would stop working. And then you would have two problems: You would have your pain, and you would be dependent on this drug and experience painful withdrawal if you try to get off [opioids].
Clearly, it’s time for members of the American medical community to seek safer alternatives. Some are doing just that.
Alternatives to Opiates
In January of 2016, a hospital in Patterson, New Jersey — with the state’s largest ER — decided to take action. That’s when the staff at St. Joseph’s Regional Medical Center instituted a groundbreaking program called ALTO (Alternatives to Opiates).
 The program was founded Dr. Mark Rosenberg, the hospital’s emergency department chairman. After seeing so many individuals struggle with the consequences of opioid use, he wanted to offer his patients some alternatives.
The program was founded Dr. Mark Rosenberg, the hospital’s emergency department chairman. After seeing so many individuals struggle with the consequences of opioid use, he wanted to offer his patients some alternatives.
And he’s been successful. In the first two months of the program, 75% of the 300 hospital’s ER patients left the hospital without opioids. After five months, they had reduced opioid use in the Emergency Department by 38%.
For some, the alternative provided was the safe and short-term administration of nitrous oxide (“laughing gas”). It alleviates stress and creates a window of time for pain to subside naturally. ALTO also uses targeted anti-inflammatory medications (such as ibuprofen), trigger-point injections, and ultrasound-guided nerve blocks.
The team has successfully treated patients with acute pain diagnoses that run the gamut from severe headache, bone fractures, and kidney stones, to back pain and other muscular or skeletal pain. After discharge, they typically recommend that their patients seek pain management through physical therapy and acupuncture.

The hospital’s pain management program still keeps opioids available as an option, but they seek to use the alternatives first.
Non-Medication Options
Other pain management methods which medical practitioners are using to lessen reliance on opioids include:
Biofeedback
With biofeedback, individuals learn to monitor body experiences that are usually outside of their awareness, like heart rate or blood pressure. In the case of pain, patients are taught to look for cues of their discomfort, become more aware of their symptoms, and adapt to control them.
 For instance, by identifying tight muscles and learning to relax those muscles, biofeedback can help relieve lower back pain, abdominal pain, TMJ and fibromyalgia. One study showed biofeedback to be effective in reducing upper-body pain in up to 86 percent of adult patients.
For instance, by identifying tight muscles and learning to relax those muscles, biofeedback can help relieve lower back pain, abdominal pain, TMJ and fibromyalgia. One study showed biofeedback to be effective in reducing upper-body pain in up to 86 percent of adult patients.
Hypnotherapy
Hypnotherapy is another technique to help relieve pain without the use of medication. In theory, hypnosis works by making patients aware of the source of their pain, underlying issues that make it worse, and the ways they can better manage it.
During hypnosis, the patient often becomes more open to specific suggestions and goals, such as reducing pain.
In 1996, a panel at the National Institutes of Health found hypnosis to be effective in easing cancer pain. More recent studies have also demonstrated its effectiveness for pain related to burns, and rheumatoid arthritis. An analysis of 18 studies by researchers at Mount Sinai School of Medicine in New York support the effectiveness of hypnotic techniques for pain management.
Hypnosis and biofeedback have been shown to be about equally effective in relieving lower back pain.
 Cognitive Behavioral Therapy
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy ( or CBT) helps alleviate pain and depression by identifying dysfunctional thoughts or attitudes and developing coping mechanisms. With CBT patients suffering from chronic pain can control their perceptions of pain by:
- Realistically evaluating the effect of the pain and how long it will last
- Learning strategies to adapt to their symptoms (rather than catastrophizing, or thinking about their pain in a dramatic, extreme, or hopeless manner
This approach, in turn, reduces the focus on pain. By changing their negative thoughts and behaviors, patients can change their awareness of pain and develop better coping skills, even if the actual level of pain stays the same.
CBT can also change the physical response in the brain that makes pain worse. In control group studies, CBT has proven to be at least as good or better than other pain treatments.
What Does the Future Hold?
We now know that chronic pain actually alters brain chemistry. Which is why the future of pain management will likely focus on the biggest player in the way we experience pain: The Mind.
Take a look:
Sources:


Trackbacks/Pingbacks